“Anxious and angry relatives are a burden all doctors must bear, but having been one myself was an important part of my medical education.”
― Henry Marsh, Do No Harm: Stories of Life, Death and Brain Surgery1
Accusing finger
“Doctors in India are not as effective as those abroad!” This was Jogi’s son, GG.
His casual statement stung me.
Jogi (Dr Joginder Singh), an old friend, had worked all his life as a physician in the public sector and had joined a private hospital after superannuation.2
Jogi was a doting father, who had allowed his son to study the subjects as he liked. In his younger days, GG loved sports but was not particularly good at playing any. He finally ended up doing a Bachelor of Physiotherapy (BPT). Jogi had at this stage, channelled him into doing a Master of Public Health (MPH). Now he had applied for a WHO job and was waiting for results to be announced.
After his MPH, GG had started making some head-turning observations. Jogi supported him as a general rule, in whatever he said.
I retorted. ” Don’t talk through your turban! How can you make such unscientific claims which will demoralise our already dispirited clan!”
Jogi calmly replied, “ Oh AC, he is talking through a natural orifice and just hear him out.”
“Okay, prove it. Do you even know what effectiveness means for a doctor?” I challenged him.
What is effectveness?
GG had a mischievous look in his eyes, “At a basic level, the effectiveness of a doctor means his/her ability to see, communicate with, diagnose, and treat an individual patient to the latter’s satisfaction.”3
It was simple and straight. But I asked, “What are the other levels?”
“Of course!” He replied, “The next level is that of communicating and working effectively with local colleagues of various specialities. And then there are other levels of collaboration with health workers at the regional and national levels.”
“I will accept that, but which level are you talking about?”
“I think, it is best to begin at the basic level. Higher levels would involve a structured organisation, like NHS in the UK, which is somewhat lacking in India.”
“Okay!why are Indian doctors ineffective?” I waited for him to go on.
“Uncle, let me begin by telling you a historical anecdote about Alexander and his physician Philip.” GG said.
I again challenged, “Stories will not be taken as evidence!”
“Just listen.” Jogi intervened.
Legend of Alexander the Great
GG Said, “It is a documented historical fact that once Alexander had become severely ill when his army was passing through Cilicia in 333 B.C.4 The court’s physicians were afraid to treat him, as they were wary of the potential adverse consequences of a failed treatment. A new physician named Philip “the Acarnanian,” was called in. However, when Philip was about to administer the treatment, Alexander received a message from Parmenion, one of his greatest generals, informing him that Philip had been bribed by the Persian King Darius III to poison him in guise of treatment.”
I asked, “What did Alexander do?”
GG carried on, “Notwithstanding this, Alexander kept his trust in Doctor Philip and drank the medicine prepared by his physician. Alexander recovered soon to fight another war. This anecdote has been immortalised in the painting by the Polish master Henryk Siemiradzki (See below)”
“Hmmm.” I wondered what he wanted to convey, when Jogi said, “GG is trying to underline the importance of patient’s trust in the doctor!”

GG went on, “For a doctor to be effective, the patient must have trust in him! This is an accepted fact of our profession.5,6,7
The evidence
“I agree” I knew he was right.But Jogi added to support his son, “You wanted evidence? There is a metanalysis that shows that healthcare outcomes are significantly better when trust levels are high.”8
GG commented, “In India, doctors have lost the trust of their patients. That majorly hampers the efficacy of doctors at the basic level. In the West, however, doctors are one of the most trusted professionals, including Indian doctors working there.”9,10
I knew he was right, but asked anyway, “Why is trust so important?”
GG was an expert now, “I will give you two closely related reasons.”
I looked on expectantly.
GG said, “Firstly patients lose the benefit of the placebo effect!”11,12
I was surprised that he knew about the placebo effect. “How do you know about the placebo effect?”
He answered, “In medical research, it is a well-known fact. When clinical trials are conducted, the group of patients who receive a dummy tablet (i.e. control group) get no treatment but show good improvement in 30-50% cases.13 In fact, the doctor’s belief in medicine also increases patient’s response!”
I knew that he was right. “And what is the second reason.”
Nocebo effect
GG said, “Second is the opposite of placebo effect, and is called the nocebo effect.”14,15
And without my asking, he went to describe it. ” Nocebo response happens when a person’s negative expectations of treatment lead to excessive side effects. And one of the outcomes is that up to 50% of patients do not take medicines as prescribed.”16
Jogi added his own philosophy to support GG. “AC, the power of the human mind has not been fully understood. I remember a movie “Taare Zameen Par”17 in which a dyslexic child was told about an interesting legend. According to this story, in the Solomon Islands of the Pacific, the islanders practise a special form of curse magic. If a tree needs to be cut down and is too big to be chopped down, it is brought down by the combined efforts of the islanders cursing negatively and yelling at the tree. This negative energy somehow damages the tree’s life. The result is that after about 30 days of getting cursed the tree dies off and falls to the ground! Looks like ‘nocebo effect’ to me.”
I said, “Jogi, I don’t know if it has been scientifically proven? But I agree with GG that the human mind has tremendous, I would say, unfathomable influence on the human body. It is being explored in a new branch of science called psycho-endo-neuro-immunology.”18
Jogi added, “I agree with you. People have willed themself to die or even cure cancers!”19,20,21,22,23,24, 25
Why has it happened?
I asked GG, “Pray, can you tell me, why doctors in India have lost the trust of patients?”
GG replied, “There are several papers written on this subject.”26,27, 28,29 59, 30 “The main reason is difference in perceptions of patients and doctors.”
Table to summarise GG’s theory
| Public perceptions | Doctor’s response |
| Doctor’s charge exorbitant fees | Less than 10% of what patient pays in corporate hospitals goes to doctors. Rest of the money is overhead charge of hospitals. |
| Doctors prescribe large number of tests | For making a clinical diagnosis with 50-70% accuracy, very few tests are needed, But to increase accuracy to 75-90% several additional investigations are required. Moreover, many drugs can cause excessive side effects in patients with pre-existing disease, hence screening tests are indicated. |
| Doctors write expensive drugs | Drug prices are not controlled by doctors. Sometimes the same drug is available in both, cheaper and expensive brands. The patient can always request doctors/pharmacists for cheapest brands, but it may not give the same guarantee of efficacy as more expensive brands do. |
| Doctors have become commercial | It is the society that has started calling the vocation of medicine as a health-care-industry. It was ab-initio the Government’s decision to equate medical consultation with business and bring it under the consumer protection act. The act suggested that patient is a consumer and the doctor is marketing/selling services. Hence, the rules of business were introduced. Private medical colleges charge exorbitant fees and doctors have to take huge loans to complete their education, which need to repaid timely. |
| There is a nexus between doctors and pharmaceutical industry | Doctors are victims of very aggressive marketing. Just as the public consumes harmful cold drinks and cosmetics due to aggressive marketing, doctors also fall a prey. |
| We have to search for a good doctor on mobile apps just as we search for restaurants on mobile apps. But rating are not reliable | Third-party apps have to earn money and therefore they often give paid ratings |
| Doctors don’t have time for patients | Time is dependent on doctor-patient ratio. Patient loads are high in India. Then there are many mandates imposed on doctors that affect patient care, for example, extensive documentation and paperwork. There is always a large number of patients to be seen. Time spent with each patient, therefore, is perforce limited. |
| Doctors are corrupt | Outlier doctors have been gaming the system. Most doctors truly put patients’ care first, before profit. But, there are a few who inappropriately use their medical degrees for profit. |
| Everyone is critical of the medical profession | The majority of doctors are honest and dedicated to patient care. They are equally distressed at media maligning their reputation. There are big stories about the pill mill doctors and those arrested for fraud or harassment. There are so many more amazing stories of heroic doctors among us than the bad apples. But the press does not give them attention. People rather see the bad than the good. This too tends to paint us all in a negative light. |
Lack of trust in doctor-patient relationship can be explained by different perceptions about existing situation by patients and doctors..
Jogi added, “You have also written somewhere that, the public today has to make a choice between state-run monoliths and corporate mercenaries!”31
Are Doctors the main culprit?
I confessed, “I have no doubt that trust is the cornerstone of any relationship and more so for the doctor-patient relationships. But the question is how do we bring in the trust?”
GG drove his point further, “The last decade has seen doctors in India being increasingly exposed and indicted on counts of corruption, professional negligence, taking kickbacks, and illegal dual practice, both in the court of law and in the society at large.32,33,34,35 Even the Medical Council of India, the statutory body responsible for overseeing the ethical conduct of doctors is seen as a corrupt body.36,37,38
Jogi joined the chorus,” Remember Parliamentary Committee report saying- the Medical Council of India … has repeatedly failed on all its mandates over the decades, and that the state of the medical profession is perhaps at its “lowest ebb.”39
“But Jogi, you must also remember the other words of the same report.” I protested and quoted, “This erosion of trust is not …..unique to the medical profession in India; evidence shows that it is a growing concern, globally,40,41 and the Indian situation has parallels in many low- and middle-income country (LMIC) health systems.42, 43,44
GG said, “But I think, it is not as bad as in India!”
What can we do now?
I again retorted, “Let’s not be a sanitary inspector and stop at saying everything is dirty. How do we improve the situation? Personally, I feel, trust should also not be blind as is seen in some villagers coming to big cities. It should be conditional and appropriately earned to avoid exploitation.”45
Jogi nodded. ” You would not approve of Alexander trusting his physician Philip?”
I ignored him and went on further,” One must also clearly differentiate between trust in a particular doctor and trust in an institution!”
GG surprisingly was enthusiastic about this concept,” Yes, we call the latter as ‘systems trust’, and it signifies accountability and the checks and balances in the systems that maintain fairness, preventing incompetence or malign intent.”46
I hammered on,” So what we have is a lack of systems trust due to failure of MCI guided stewardship of the medical profession. As a few studies have indicated, a patient may distrust the medical profession as a whole but may still maintain trust in his/her personal physician on an individual basis.”47,48,49
Jogi also agreed with me, “Yes many of my patients trust me and have been with me for nearly 20 years.”
MCI to NMC
GG raised another doubt, “But the question is, will the change of name from MCI to NMC make much of a difference?”50,51
I said,” The systems approach by National Health Service (NHS) in the UK, has also not been a great success.”52
GG added his bit,” We need a two-pronged approach. On one hand, robust and fair control-based interventions by the NMC is required which will improve the transparency, and accountability, in professional practice. On the other hand, initiatives are required which encourage and maintain the trusting interpersonal relations between patients and their providers.”
Jogi asked, “A few years back a white paper was published to outline measures for rebuilding patient-physician trust in China. Any success with that?”53
I said, “Many such recommendations have been made.54,55,56
GG informed us, “NMC has also taken several steps. For example, they have implemented competency-based medical education in all medical colleges with the addition of courses on medical humanities and medical ethics.”
Patients and doctors, both are losers
I remarked, “Morality cannot be learnt in the classroom. Would people learn morality after paying a hefty fee for admission to private medical colleges? Isn’t the financial pressure of loan repayment a hindrance to altruistic work?”
GG laughed, “Yes, there are many theories, little data and fewer measures to improve trust.”57
Jogi deviated from his usual pattern of response and said, “GG, your stance suggests that doctors are ineffective and patients are distressed because of either the patient’s fault (lack of trust) or organisational failure on part of MCI. Doctors themselves are the holy cows, who can never be wrong!”
I had to speak for doctors, “Doctors come from the same stock as the general public, but that is no defence for some of the immoral things that doctors are accused of doing. It is for us to realize that ours is a vocation, and not a business as some administrative rules seem to suggest. The trust can only be built over time when our conduct remains above suspicion. Many in our fraternity lack soft skills and need to undergo intensive training in subjects such as ‘how to break the bad news, ‘how to deal with difficult patients’ and ‘evidence-based care’. Doctors should also take time to justify to patients the scientific rationale of their action.”
Jogi remarked, “Don’t you think, various associations of doctors need to revisit their policies of holding ostentatious meetings with glitzy evening entertainment programmes. Doctors also need to educate themselves about how the pharmaceutical industry manipulates them. Overall, they need to do what everyone should, i.e. control their greed and act responsibly. The regulatory body with transparent functioning needs to take care of the bad sheep in the profession.”
I could not agree more. GG too had a suggestion,” Corporate hospitals today pay private practitioners to get more referrals and encourage ‘cut practice’. If it is unethical for a doctor to receive such money, it should also be so for a hospital. To discourage such practices, corporate hospitals should be asked to justify costs and their billing process must be scrutinized by the regulatory bodies.”
Suggestions welcome
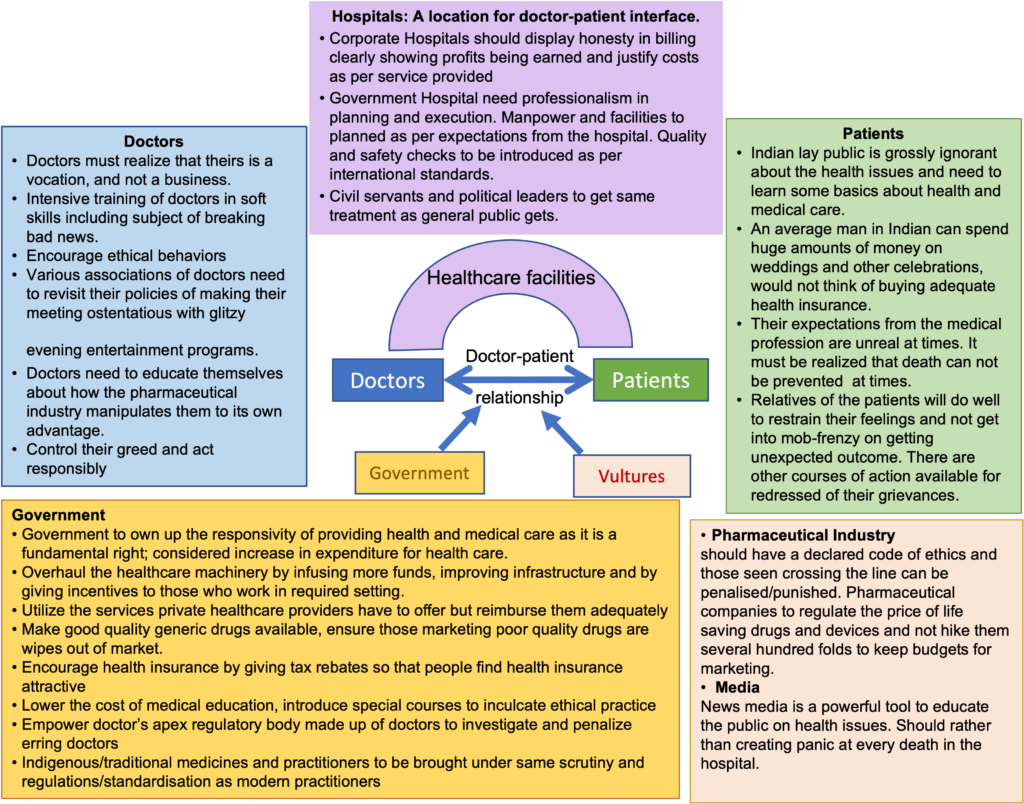
Jogi turned to GG and pushed a magazine towards him, “ AC’s views are already published. (See figure-2 below)”58 GG, what is new that you would like to add?”
GG fumbled for a few seconds and said, “Why don’t we ask the doctor fraternity and the lay public at large?”
And that is how the matter has been brought before you! Your turn now to suggest new innovative ideas!
Authors note: The names of characters are fictitious, while issues are real. The last figure and several quotations are from my papers published in National Medical Journal of India. The author is grateful to the editor for permitting him to use this material for this blog.
References
| ↑1 | https://www.goodreads.com/work/quotes/40447706-do-no-harm-stories-of-life-death-and-brain-surgery |
| ↑2 | Anand AC. Swami Ramdev and scientific medicine: losing is fine, but the lesson should not be lost! Natl Med J India. 2007 Sep-Oct;20(5):256-9. PMID: 18254525. |
| ↑3 | Davies P. The levels of medical effectiveness. Br J Gen Pract. 2009;59(566):702-703. doi:10.3399/bjgp09X454269 |
| ↑4 | Vilela E, Fontes-Carvalho R. Alexander the Great Trusts Doctor Philip: The Patient-Physician Relationship as the First Step of the Healing Process. JACC Case Rep. 2020 Jul 15;2(8):1229-1231. doi: 10.1016/j.jaccas.2020.05.080. PMID: 34317456; PMCID: PMC8311878. |
| ↑5 | Pellegrini CA. Trust: The Keystone of the Patient-Physician Relationship. J Am Coll Surg. 2017 Feb;224(2):95-102. doi: 10.1016/j.jamcollsurg.2016.10.032. Epub 2016 Oct 20. PMID: 27773776. |
| ↑6 | David H Thom, Richard L Kravitz, Robert A Bell, Edward Krupat, Rahman Azari, Patient trust in the physician: relationship to patient requests, Family Practice, Volume 19, Issue 5, October 2002, Pages 476–483, |
| ↑7 | Krot, K., Rudawska, I. (2016), The Role of Trust in Doctor-Patient Relationship: Qualitative Evaluation of Online Feedback from Polish Patients, Economics and Sociology, Vol. 9, No 3, pp. 76-88. DOI:10.14254/2071-789X.2016/9-3/7 |
| ↑8 | Birkhäuer J, Gaab J, Kossowsky J, Hasler S, Krummenacher P, et al. (2017) Trust in the health care professional and health outcome: A meta-analysis. PLoS ONE 12: e0170988. |
| ↑9 | https://www.fiercehealthcare.com/practices/survey-finds-over-9-10-people-say-doctors-are-most-trusted-professionals |
| ↑10 | https://blogs.library.duke.edu/rubenstein/2019/10/02/why-do-we-trust-doctors/ |
| ↑11 | Kaptchuk TJ, Miller FG. Placebo Effects in Medicine. N Engl J Med. 2015 Jul 2;373(1):8-9. doi: 10.1056/NEJMp1504023. PMID: 26132938. |
| ↑12 | Meissner K, Kohls N, Colloca L. Introduction to placebo effects in medicine: mechanisms and clinical implications. Phil. Trans. R. Soc. B. 2011;366:1783-9. |
| ↑13 | Del Re AC, Maisel N, Blodgett JC, Wilbourne P, Finney JW. Placebo group improvement in trials of pharmacotherapies for alcohol use disorders: a multivariate meta-analysis examining change over time. J Clin Psychopharmacol. 2013;33(5):649-657. doi:10.1097/JCP.0b013e3182983e73 |
| ↑14 | Planès S, Villier C, Mallaret M. The nocebo effect of drugs. Pharmacol Res Perspect. 2016;4(2):e00208. Published 2016 Mar 17. doi:10.1002/prp2.208 |
| ↑15 | Faasse K, Petrie KJThe nocebo effect: patient expectations and medication side effectsPostgraduate Medical Journal 2013;89:540-546. |
| ↑16 | Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005 Aug 4; 353(5):487-97. |
| ↑17 | https://www.manochikitsa.com/power-of-subconscious-mind/ |
| ↑18 | Tausk F, Elenkov I, Moynihan J. Psychoneuroimmunology. Dermatol Ther. 2008 Jan-Feb;21(1):22-31. doi: 10.1111/j.1529-8019.2008.00166.x. PMID: 18318882. |
| ↑19 | https://www.bbc.com/future/article/20150210-can-you-think-yourself-to-death |
| ↑20, ↑23 | https://qz.com/1407287/giving-up-on-life-can-lead-to-actual-death-in-less-than-a-month/ |
| ↑21, ↑24 | https://www.bbc.com/future/article/20150306-the-mystery-of-vanishing-cancer |
| ↑22, ↑25 | https://med.stanford.edu/survivingcancer/cancers-existential-questions/cancer-will-to-live.html |
| ↑26 | Kane S, Calnan M. Erosion of Trust in the Medical Profession in India: Time for Doctors to Act. Int J Health Policy Manag. 2017;6(1):5-8. Published 2017 Jan 1. doi:10.15171/ijhpm.2016.143 |
| ↑27 | <a href=”https://www.physiciansweekly.com/doctors-losing-publics-trust/ |
| ↑28 | https://www.firstpost.com/india/violence-against-doctors-growing-trust-deficit-with-patients-at-core-of-medical-systems-rot-policymakers-must-act-quickly-7562611.html |
| ↑29 | https://www.physiciansweekly.com/doctors-losing-publics-trust/ |
| ↑30 | https://www.newindianexpress.com/thesundaystandard/2018/mar/11/doctors-meet-discusses-loss-of-trust-by-patients-1785163.html |
| ↑31 | Anand AC. Indian healthcare at crossroads (Part 1): Deteriorating doctor-patient relationship. Natl Med J India. 2019 Jan-Feb;32(1):41-45. doi: 10.4103/0970-258X.272117. PMID: 31823941. |
| ↑32 | Jain A, Nundy S, Abbasi K. Corruption: medicine’s dirty open secret. BMJ. 2014;348:g4184. doi:10.1136/bmj.g4184 |
| ↑33 | Bawaskar HS. The medical trade. Indian J Med Ethics. 2013;10(4):278. |
| ↑34 | Sachan D. Tackling corruption in Indian medicine. Lancet. 2013;382(9905):e23-e24. |
| ↑35 | Jesani A. Professional codes, dual loyalties and the spotlight on corruption. Indian J Med Ethics. 2014;11(3):134-136. |
| ↑36 | Mani MK. Our watchdog sleeps, and will not be awakened. Issues Med Ethics. 1996;4(4):105-107. |
| ↑37 | Chatterjee P. Trouble at the Medical Council of India. Lancet. 2010;375 (9727):1679. doi:10.1016/S0140-6736(10)60720-9 |
| ↑38 | Vijayakumar K, Saini N. Medical Council of India in a constitutional crisis. J Indian Med Assoc. 2013;111(10):706. |
| ↑39 | The functioning of Medical Council of India. Department-related parliamentary standing committee on health and family welfare (Report No. 92). India: Parliament of India; March 2016. |
| ↑40 | Blendon RJ, Benson JM. Public trust in physicians – U.S. medicine in international perspective. N Engl J Med. 2014;371:1570-1572. doi:10.1056/NEJMp1407373 |
| ↑41 | Timmermans S, Oh H. The continued social transformation of the medical profession. J Health Soc Behav. 2010;51(1):S94– S106. doi:10.1177/0022146510383500 |
| ↑42 | Tucker JD, Cheng Y, Wong B, et al. Patient-physician mistrust and violence against physicians in Guangdong Province, China: a qualitative study. BMJ Open. 2015;5:e008221. doi:10.1136/ BMJ open-2015-008221 |
| ↑43, ↑45 | Tucker JD, Wong B, Nie J, Kleinman A. Rebuilding patient–physician trust in China. Lancet. 2016;388(10046):755. doi:10.1016/S0140-6736(16)31362-9 |
| ↑44 | Okello DRO, Gilson L. Exploring the influence of trust relationships on motivation in the health sector: a systematic review. Hum Resour Health. 2015;13:16. doi:10.1186/s12960- 015-0007-5 |
| ↑46 | Kane S, Calnan M. Erosion of trust in the medical profession in India: time for doctors to act. Int J Health Policy Manag. 2017;6(1):5–8. doi:10.15171/ijhpm.2016.143 |
| ↑47 | Kane S, Calnan M, Radkar A. Trust and trust relations from the providers perspective: the case of the health care system in India. Indian J Med Ethics. 2015;12(3):157-168. |
| ↑48 | Gopichandran V, Chetlapalli SK. Factors influencing trust in doctors: a community segmentation strategy for quality improvement in healthcare. BMJ Open. 2013;3:e004115. doi:10.1136/bmjopen-2013-004115 |
| ↑49 | Baidya M, Gopichandran V, Kosalram K. Patient-physician trust among adults of rural Tamil Nadu: a community-based survey. J Postgrad Med. 2014;60:21-26. |
| ↑50 | Nagral N, Jain A, Nundy S. A radical prescription for the Medical Council of India: hope for a cure. BMJ. 2016;352:i1731. doi:10.1136/bmj.i1731 |
| ↑51 | Mollering G. The Trust/Control Duality: an integrative perspective on positive expectations of others. Int Sociol. 2005;20:283. doi:10.1177/0268580905055478 |
| ↑52 | Brown P, Calnan M. The civilizing process of trust: developing quality mechanisms which are local, professional-led and thus legitimate. Soc Policy Adm. 2011;45(1):19-34. |
| ↑53 | Tucker JD, Wong B, Nie J, Kleinman A. Rebuilding patient–physician trust in China. Lancet. 2016;388(10046):755. doi:10.1016/S0140-6736(16)31362-9 |
| ↑54 | Rolfe A, Cash-Gibson L, Car J, Sheikh A, McKinstry B. Interventions for improving patients’ trust in doctors and groups of doctors. Cochrane Database Syst Rev. 2006;(3):CD004134. doi:10.1002/14651858.CD004134.pub3 |
| ↑55 | Bachman R, Gillespie N, Priem R. Repairing trust in organizations and institutions: Toward a conceptual framework. Organ Stud. 2015;36(9):1123-1142. doi:10.1177/0170840615599334 |
| ↑56, ↑58 | Anand AC. Indian healthcare at crossroads (part 3): Quo vadis? Natl Med J India. 2019 May-Jun;32(3):175-180. doi: 10.4103/0970-258X.278696. PMID: 32129315. |
| ↑57 | Pearson SD, Raeke LH. Patients’ trust in physicians: many theories, few measures, and little data. J Gen Intern Med. 2000 Jul;15(7):509-13. doi: 10.1046/j.1525-1497.2000.11002.x. PMID: 10940139; PMCID: PMC1495476. |
| ↑59 | https://www.firstpost.com/india/violence-against-doctors-growing-trust-deficit-with-patients-at-core-of-medical-systems-rot-policymakers-must-act-quickly-7562611.html |
Yet another masterpiece on an important issue concerning various stakeholders in healthcare provisioning. Different perspectives of all have been very appropriately highlighted. Bright and sunny day augmented by a brilliant and enriching scientific input.
Thanks for sharing Sir
Many doctors who practice or are employed in Corporate hospitals have not done MBBS. However, many patients do not know the difference between an MBBS doctor or those who have done a course in alternate medicine.
Secondly, in many places, patients relatives have behaved violently with doctors. Surprisingly, the other patients do not defend the doctors.
Lastly, if they feel that doctor A is ineffective, they can go to a doctor B. Or to the alternate medicine doctor.
Excellent article.Beautifully brouhhforth present day Lacunae and challenges of Indian Medical practice