“In a fast, the body tears down its defective parts and then builds anew when eating is resumed.”
― Herbert M. Shelton, Fasting for Renewal of Life
Current COVID-19 pandemic has pushed into relative obscurity, another pandemic that has been raging for over one decade.1 By confining people to their homes, COVID-19 may make that pandemic of obesity worse. So any simple treatment that promises a dramatic benefit, evokes great excitement. A recent paper published in a popular journal dealt with one such simple measure i.e. intermittent fasting (IF).2 It also brought back some forgotten memories from my childhood.
I was seven years old then. My father had brought his maternal aunt (Massiji) to live with us. She was 97 years old, bent at her waist and walked with the help of a stick. She became my roommate as both of us had our beds in a small room that was called the storeroom. I was delighted with the new company for two reasons. I loved her toothless smile, especially laughter and found the stories of her childhood very amusing.
My mother wasn’t too happy with this development as it escalated her workload significantly. Every other day, Massiji (that’s what we all started calling her) would want to observe a religious fast and my mother had to cook special ‘vrat’ food for her before sunrise. I often asked Massiji,”why are you fasting today?” And every time her answer would be different – ‘It’s ekadashi today’ or ‘its sankranti today,’ or ‘its chaturthi today,’ and so on. My impression at that age was that Massiji did all this just to impress upon every one that she deserved this fuss because she was a senior member in the household. Maybe my thoughts were influenced by listening to my mother’s misgivings about her demeanour.
After I became a physician, I often came across papers stating that the people who fast, live longer.3,4 But such papers are usually considered amusing stories and fall on the collective blind spot of the medical community. Academic circles are always more busy with endeavours to find new treatments for diseases such as obesity, diabetes mellitus and non-alcoholic fatty liver disease (NAFLD) as these had assumed pandemic proportions.5,6,7
As a Gastroenterologist, I have attended numerous conferences on the NAFLD, where the main focus was on the molecular mechanisms underlying this disease and the new drugs being developed to block ‘x’ or ‘y’ pathways inside a cell.8 The simple fact that exercise and weight loss could cure most patients9 was discussed for less than 5% of time during these conferences. Organisers confessed that no drug companies were willing to sponsor the time to discuss exercise and diet! I have often vocalised my reservations at these conferences, “Why do we focus only on the newer, less effective and more toxic treatments, when a free and universally effective treatment was available.” But my interjections were politely sidelined as conferences went about discussing, with great enthusiasm, a recently developed drug that would benefit 4% patients over and above the numbers that were benefited by a placebo (Though half the patients treated will have side effects!).10
I too, have been overweight for over two decades now. I know that I need to lose weight.I have tried vigorous diet+exercise programmes several times in my life, with good results too. The minute my attention went to some other activity or event in my life, the weight would came back quickly. I realise that eating stimulates the same pleasure centers that alcohol does.11 The effects of overeating and alcohol on the liver are also very similar. So all obese people who are unable to loose weight really need de-addiction programmes and support groups rather than more drugs. Our efforts should be directed towards motivating people to stick to a healthy lifestyle rather than developing new drugs to control obesity. Governments can intervene with measures to target eating behaviours by introducing curbs on the marketing and availability of unhealthy food choices, and imposing physical constraints on food.12 Action plans as suggested for Poland13 are required everywhere. In this light, the paper I mentioned earlier,14 was a timely reminder of an easy solution available for our problems. But is there scientific evidence to support it?
Basic physiology of intermittent fasting (IF) is very simple. Feeding leads to increased insulin secretion, which is an anabolic hormone. It’s action results in deposition of extra glucose as glycogen, and fat as triglycerides in adipose tissues. Human cells sense abundance as there is accumulation of energy storing molecules.15 The protein/ amino acid abundance stimulates the activity of mTOR,47 resulting in enhanced protein synthesis and cell growth.
Energy restriction (fasting) for 10 to 14 hours or more results in depletion of liver glycogen stores and mobilisation of fat from adipose tissue. Body switches from glucose based energy extraction to fat based energy extraction (popularly called the metabolic switch).16 Triglycerides are hydrolysed to free fatty acids(FFAs) in fat cells (adipocytes) and are transported to the liver, where they are converted to the ketone bodies(KBs), acetoacetate and β-hydroxybutyrate (β-HB).
- β-HB and acetoacetate can be utilized in the Krebs cycle to generate energy. β-HB also has intracellular signaling functions for activation of various transcription factors in neurons.17
- FFAs too activate the transcription factors with widespread effects on cells throughout the body and brain.18
- Reduced levels of glucose and amino acids during fasting result in reduced activity of the mTOR pathway and up-regulation of autophagy.19
The depletion of the bioenergy sensors, and activation of transcription signals lead to minimizing anabolic processes (synthesis, growth, and reproduction). On the other hand, there is an attempt to preserve the maintenance and repair systems, enhancing stress resistance, recycling damaged molecules, stimulating mitochondrial biogenesis, and promoting cell survival. All these effects support improvements in health and disease resistance.20
In the fed state, blood levels of ketone bodies are low, and in humans, they rise within 8 to 12 hours after the onset of fasting, reaching levels as high as 2 to 5 mM by 24 hours.21 The timing of this response gives some indication of the appropriate periods of fasting required in IF regimens.22 In humans, the three most widely studied IF regimens are as follows:
- Alternate-day fasting: complete fasting (water only) every other day. It appears to be the toughest regime. Less severe form of this regimen will allow 25% of average daily consumption of Calories to be allowed on the ‘fast’ day.
- 5:2 Intermittent Fasting (i.e. fasting 2 non-consecutive days each week).23 It is a relatively simpler regimen as on the fast day one could take upto 500 Cal with black coffee and unrestricted water. Other five days are for normal food (minus refined carbohydrates).
- Daily time-restricted feeding. (two meals 6-8 hours apart followed by fast of 16-18 hours),24,25 This is also relatively simple as one is required to skip one major meal -either breakfast or dinner. Snacking has to go in all the regimes.
Diets that markedly reduce caloric intake on 1 day or more each week (e.g., a reduction to ~500 calories per day) result in elevated levels of ketone bodies on those days indicating the metabolic switch from the use of glucose as a fuel source to the use of fatty acids and ketone bodies.26,27,28
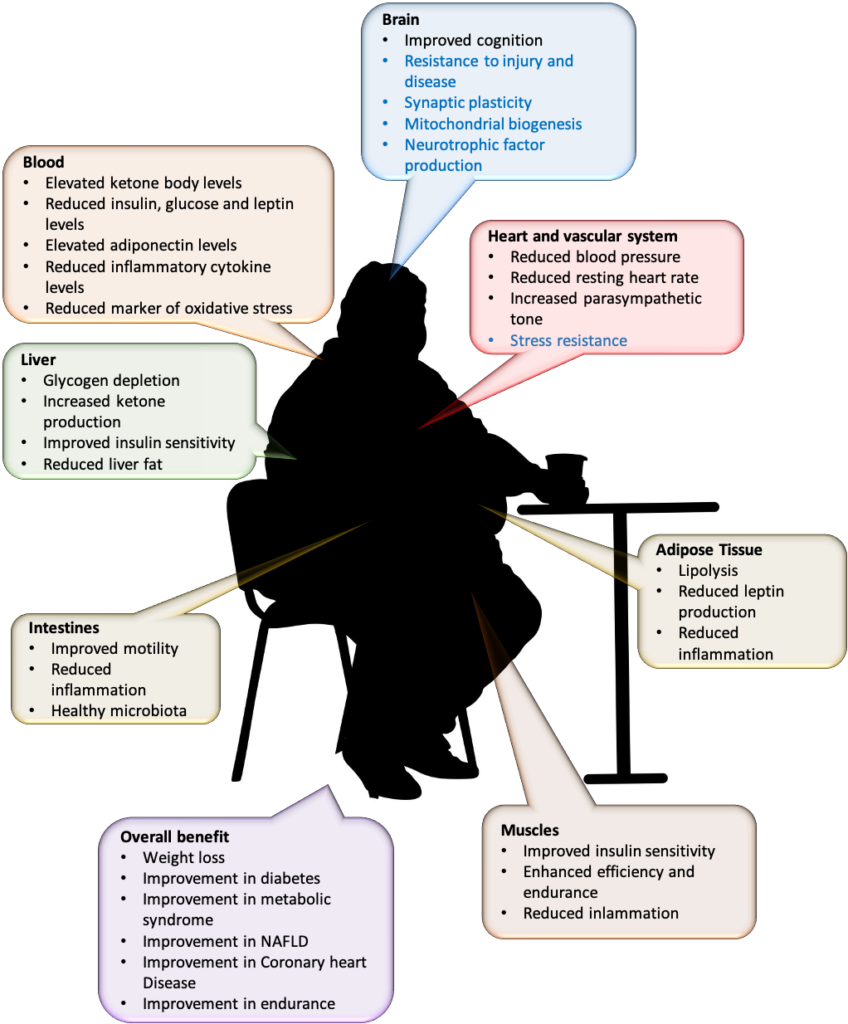
Benefits of IF have been proven in many studies and are summarised in the figure below. Benefits are as strong as you would get by permanently cutting down your calorie intake by ~30% in all meals, which remains an option. These benefits include weight loss, improvements in glucose regulation, blood pressure, and heart rate; the efficacy of endurance training and abdominal fat loss.29
The big question is, ‘Will there be side effects?’ Well, many people do report experiencing hunger, irritability and reduced ability to concentrate in the beginning. These side effects disappear within one month or so.31,32,33 A special group deserves separate mention as the diabetic patients on medications are especially scared of fasting due to risk of hypoglycaemia. But IF is important for them too because IF can cure type-2 diabetes!34,35,36 There is potential risk of hypoglycaemia in those who are on certain medicines such as insulin and sulphonylureas (including the short-acting meglitinides). In this group IF needs to be supervised.37,38,39 Doses of these drugs may need to be readjusted with shorter acting drugs used according to the meal timing.40
Most convenient may be 5:2 IF, i.e. fast on two non-consecutive days in a week with reducing food intake to 25% of daily intake (~500 Cal/day) on the fasting days.41 Oral anti-diabetic medicines that can cause hypoglycaemia can be skipped on the fasting days and insulin dose reduced to only basal dose. Water can be taken during the fasting period unrestricted. People who should refrain from IF include pregnant and lactating women, young children, adults who are frail or have a systemic acute or chronic disease, and Individuals with immunodeficiencies, including those who have had a solid organ transplant and are on medical immunosuppression.
If you are wondering what all can I eat within 500 Calories, there is a wealth of information available.42,43,44,45
In contrast to our current practice, our human ancestors did not consume three regularly spaced large meals, plus snacks, every day, nor did they lead a sedentary life. Homo sapiens in their natural habitat were supposed to struggle the whole day to get food. Evolution of the brain, language, imagination and creativity has led to development of technology to make us comfortable. As a result we have gradually transformed into the present lazy, scheming and eating-for-pleasure versions of ourselves.46 For Indians, IF comes naturally as it is our ancient wisdom. It is now being marketed commercially as a magical treatment of obesity and metabolic syndrome.
Now I understand that my impressions about my Massiji were utterly wrong. So were my mother’s. What Massiji did was rooted in our culture. Ancient wisdom had established these practices after years of experience. In fact, my mother, who was so critical of Massiji in those early days, herself switched to “only fruits” on Tuesday and Saturday in her middle years. And she had not even read any medical paper. It’s time I did it too.
References
| ↑1 | Berry E M. The Obesity Pandemic—Whose Responsibility? No Blame, No Shame, Not More of the Same. Frontiers in Nutrition 2020; 7: DOI=10.3389/fnut.2020.00002. Available at URL=https://www.frontiersin.org/article/10.3389/fnut.2020.00002 |
| ↑2, ↑14, ↑20 | de Cabo R, Mattson MP. Effects of Intermittent Fasting on Health, Aging, and Disease. N Engl J Med 2019; 381:2541-2551. DOI: 10.1056/NEJMra1905136 |
| ↑3 | Wei M, Brandhorst S, Selehchi M, Mirzaei H, Cheng CW, Budniak J, et al. Fasting-mimicking diet and markers/risk factors for aging, diabetes, cancer, and cardiovascular disease. Science Translational Medicine 2017; 9(377): eaai8700. DOI: 10.1126/scitranslmed.aai8700. |
| ↑4 | Patterson RE, Laughlin GA, LaCroix AZ, et al. Intermittent Fasting and Human Metabolic Health. J Acad Nutr Diet. 2015;115(8):1203-1212. doi:10.1016/j.jand.2015.02.018) |
| ↑5 | Dhatariya K. Diabetes: the place of new therapies. Ther Adv Endocrinol Metab. 2018;10:2042018818807599. Published 2018 Oct 30. doi:10.1177/2042018818807599 |
| ↑6 | Wong VW. Current Prevention and Treatment Options for NAFLD. Adv Exp Med Biol. 2018;1061:149-157. doi:10.1007/978-981-10-8684-7_12 |
| ↑7 | Khalil H, Ellwood L, Lord H, Fernandez R. Pharmacological Treatment for Obesity in Adults: An Umbrella Review. Ann Pharmacother. 2020;54(7):691-705. doi:10.1177/1060028019898912 |
| ↑8 | Cardoso, AC, de Figueiredo‐Mendes, C, Villela‐Nogueira, CA, Sanyal, AJ. New drugs for non‐alcoholic steatohepatitis. Liver Int. 2020; 40(Suppl. 1): 96– 101. https://doi.org/10.1111/liv.14354 |
| ↑9 | Hallsworth K, Adams LA. Lifestyle modification in NAFLD/NASH: Facts and figures. JHEP Reports,2019; 1 (6): Pages 468-479. https://doi.org/10.1016/j.jhepr.2019.10.008. |
| ↑10 | Intercept Announces Positive Topline Results from Pivotal Phase 3 REGENERATE Study of Obeticholic Acid in Patients with Liver Fibrosis Due to NASH.https://ir.interceptpharma.com/node/12371/pdf |
| ↑11 | Alonso-Alonso M, Woods SC, Pelchat M, et al. Food reward system: current perspectives and future research needs. Nutr Rev. 2015;73(5):296-307. doi:10.1093/nutrit/nuv002 |
| ↑12 | Mozaffarian D, Angell SY, Lang T, Rivera JA. Role of government policy in nutrition-barriers to and opportunities for healthier eating. BMJ. 2018;361:k2426. Published 2018 Jun 13. doi:10.1136/bmj.k2426 |
| ↑13 | Reducing childhood obesity in Poland by effective policies.https://www.euro.who.int/__data/assets/pdf_file/0011/350030/Reducing-childhood-obesity-in-Poland_final_WEB.pdf?ua=1 |
| ↑15 | Cells sense fed or fasting state by the ratio of energy molecules like nicotinamide adenine dinucleotide (NAD+): NADH, ATP: AMP, and acetyl CoA: CoA. These function as the bioenergetic sensors. These intermediate energy carriers activate downstream proteins that regulate cell function and stress resistance, including transcription factors such as forkhead box Os (FOXOs), peroxisome proliferator–activated receptor γ coactivator 1α (PGC-1α), and nuclear factor erythroid 2–related factor 2 (NRF2); kinases such as AMP kinase (AMPK); and deacetylases such as sirtuins (SIRTs). From reference no. 2 ibid. |
| ↑16 | Anton SD, Moehl K, Donahoo WT, et al. Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting. Obesity (Silver Spring). 2018;26(2):254-268. doi:10.1002/oby.22065 |
| ↑17 | β-HB has signaling functions, including the activation of transcription factors such as cyclic AMP response element–binding protein (CREB) and nuclear factor κB (NF-κB) and the expression of brain-derived neurotrophic factor (BDNF) in neurons. From reference no. 2 ibid. |
| ↑18 | The transcription factors mentioned are peroxisome proliferator–activated receptor α (PPAR-α) and activating transcription factor 4 (ATF4), resulting in the production and release of fibroblast growth factor 21 (FGF21), a protein with widespread effects on cells throughout the body and brain.From reference no. 2 ibid. |
| ↑19 | From reference no. 2 ibid. |
| ↑21 | Patel S, Alvarez-Guaita A, Melvin A, et al. GDF15 provides an endocrine signal of nutritional stress in mice and humans. Cell Metab 2019; 29(3): 707e8-718e8. |
| ↑22 | Di Francesco A, Di Germanio C, Bernier M, de Cabo R. A time to fast. Science 2018; 362: 770-5. |
| ↑23 | Scholtens EL, Krebs JD, Corley BT, Hall RM. Intermittent fasting 5:2 diet: What is the macronutrient and micronutrient intake and composition? [published online ahead of print, 2020 Feb 22]. Clin Nutr. 2020;S0261-5614(20)30085-6. doi:10.1016/j.clnu.2020.02.022 |
| ↑24 | Anton SD, Moehl K, Donahoo WT, et al. Flipping the metabolic switch: understanding and applying the health benefits of fasting. Obesity (Silver Spring) 2018; 26: 254-68. |
| ↑25 | Moro T, Tinsley G, Bianco A, et al. Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males. J Transl Med. 2016;14(1):290. Published 2016 Oct 13. doi:10.1186/s12967-016-1044-0 |
| ↑26 | Knopp RH, Magee MS, Raisys V, Benedetti T, Bonet B. Hypocaloric diets and ketogenesis in the management of obese gestational diabetic women. J Am Coll Nutr 1991; 10: 649-67. |
| ↑27 | Johnson JB, Summer W, Cutler RG, et al. Alternate day calorie restriction improves clinical findings and reduces markers of oxidative stress and inflammation n overweight adults with moderate asthma. Free Radic Biol Med 2007; 42: 665-74. |
| ↑28 | Harvie MN, Pegington M, Mattson MP, et al. The effects of intermittent or continuous energy restriction on weight loss and metabolic disease risk markers: a randomized trial in young overweight women. Int J Obes (Lond) 2011; 35: 714-27. |
| ↑29 | Mattson MP, Longo VD, Harvie M. Impact of intermittent fasting on health and disease processes. Ageing Res Rev. 2017;39:46-58. doi:10.1016/j.arr.2016.10.005 |
| ↑30 | Modified from Anton SD, Moehl K, Donahoo WT, et al. Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting. Obesity (Silver Spring). 2018;26(2):254-268. doi:10.1002/oby.22065 |
| ↑31 | Harvie MN, Pegington M, Mattson MP, et al. The effects of intermittent or continuous energy restriction on weight loss and metabolic disease risk markers: a randomized trial in young overweight women. Int J Obes (Lond) 2011; 35: 714-27 |
| ↑32 | Harvie M, Wright C, Pegington M, et al. The effect of intermittent energy and carbohydrate restriction v. daily energy restriction on weight loss and metabolic disease risk markers in overweight women. Br J Nutr 2013; 110: 1534-47. |
| ↑33 | Johnson JB, Summer W, Cutler RG, et al. Alternate day calorie restriction improves clinical findings and reduces markers of oxidative stress and inflammation in overweight adults with moderate asthma. Free Radic Biol Med 2007; 42: 665-74. |
| ↑34 | Klempel MC, Kroeger CM, Bhutani S, Trepanowski JF, Varady KA.Intermittent fasting combined with calorie restriction is effective for weight loss and cardio-protection in obese women.Nutr J. 2012 Nov 21; 11:98. doi:10.1186/1475-2891-11-98 |
| ↑35 | Furmli S, Elmasry R, Ramos M, Fung J. Therapeutic use of intermittent fasting for people with type 2 diabetes as an alternative to insulin. BMJ Case Rep. 2018; 2018:bcr2017221854. Published 2018 Oct 9. doi:10.1136/bcr-2017-221854 |
| ↑36 | Grajower MM, Horne BD. Clinical Management of Intermittent Fasting in Patients with Diabetes Mellitus. Nutrients. 2019;11(4):873. Published 2019 Apr 18. doi:10.3390/nu11040873 |
| ↑37 | Corley BT, Carroll RW, Hall RM, Weatherall M, Parry-Strong A, Krebs JD. Intermittent fasting in Type 2 diabetes mellitus and the risk of hypoglycaemia: a randomized controlled trial. Diabet Med. 2018 May; 35(5):588-594. |
| ↑38 | Carter S, Clifton PM, Keogh JB. Effect of Intermittent Compared With Continuous Energy Restricted Diet on Glycemic Control in Patients With Type 2 Diabetes: A Randomized Noninferiority Trial. JAMA Netw Open. 2018 Jul 6; 1(3):e180756. |
| ↑39 | Chaudhury A, Duvoor C, Reddy Dendi VS, Kraleti S, Chada A, Ravilla R, Marco A, Shekhawat NS, Montales MT, Kuriakose K, Sasapu A, Beebe A, Patil N, Musham CK, Lohani GP, Mirza W. Clinical Review of Antidiabetic Drugs: Implications for Type 2 Diabetes Mellitus Management. Front Endocrinol (Lausanne). 2017; 8:6.doi:10.3389/fendo.2017.00006 |
| ↑40 | Corley BT, Carroll RW, Hall RM, Weatherall M, Parry-Strong A, Krebs JD. Intermittent fasting in Type 2 diabetes mellitus and the risk of hypoglycaemia: a randomized controlled trial. Diabet Med. 2018;35(5):588-594. doi:10.1111/dme.13595. |
| ↑41 | Scholtens EL, Krebs JD, Corley BT, Hall RM. Intermittent fasting 5:2 diet: What is the macronutrient and micronutrient intake and composition? Clin Nutr. 2020;S0261-5614(20)30085-6. doi:10.1016/j.clnu.2020.02.022 |
| ↑42 | https://www.nriol.com/health/calorie-chart.asp |
| ↑43 | https://www.nin.res.in/downloads/DietaryGuidelinesforNINwebsite.pdf |
| ↑44 | https://www.saffrontrail.com/52-diet-all-you-need-to-know/ |
| ↑45 | http://www.eeb.cornell.edu/biogeo/nanc/Food_Feed/table%201%20gopalan%20et%20al%201989.pdf |
| ↑46 | Mattson MP. An evolutionary perspective on why food overconsumption impairs cognition. Trends Cogn Sci 2019; 23: 200-12. |
| ↑47 | mTOR stands for mammalian-target-of-rapamycin also sometimes called as the mechanistic target of rapamycin. It is a protein kinase that promotes cell and muscle growth. From reference no. 2 ibid. |
Such lucid writing, and explained so well. And I can almost visualise the toothless smile of Maasiji. What a good combination of scientific and popular styles of articulation. Pharma companies will close down for sure, if they sponsored conferences to discuss diet, weightloss, and exercise 😅. I guess, the moot point is – Only IF we could follow this 😁😁. Certainly, “It’s time I did it too.” 👍🏼 Thanks for another good post.
Excellent & Timely illustration of an most appropriate article Sir !
Dear Admiral Anand,
Very illuminating and and a highly lucid piece on the science behind IF. Drives home a very compelling case for wider adoption of IF.
If we recall the octogenarians plus in our family trees , one realizes that they were all thin individuals.
Trust me, the 16:8 IF regime is highly doable and with a tremendous feel good factor. Haven’t got into the biochemistry as yet. Besides, there is little sense of guilt on one’s “cheat” days.
Sir, really appreciate this wonderful read.
Warm regards
I find the 5:2 IF method easier and less taxing on the body (and the mind). Your style of writing is appealing and engaging at the same time (thankfully not calorific). Were you to write for a non technical audience you would be a hit (and get hits). Best wishes Sir!
another masterpiece article by the author, who has mastered the art of assimilating scientific facts & the story telling.
My sincere request to AC is to research varoios
old practices adopted by our forefathers ,hitherto thought to be only religious without any scientific basis.
The fact, modern medicine is not the panecea for all our ailments ,more so because of the life style changes.
Thanks for a great article which I really enjoyed
reading.
Not sure if you remember me.
Regards from South Africa
Ofcourse, I do. It’s a great pleasure to connect again. You’ve been one of the fittest, why would you need IF
Most lucid exposition on benefits of caloric intake suppression through Intermittent fasting scheme sir. In many Naturopathic and Ayurvedic Centres for weight loss thev are practising this by controlling intake and staggering meal times while distracting participants through aroma therapy or massage or other adjuncts.
It requires a disciplined life style to be able to carry out this strategy! Thank you for this very topical article.
There is a recent paper in JAMA which says safety in diabetes patients has not been proven. How can you say it is safe in diabetic patients?
Yes, I have also read the paper by Benjamin D Horne(i) The author is an astute researcher. He has earlier also raised doubts against IF.(ii) He has given his opinion, which is what this paper is about! Natural and cheap treatments are not easily accepted by many, particularly those supported by powerful pharmaceutical industry.
I have gone through his arguments and my thoughts are as follows:
(a) Dr Horne says: Primary focus of research has been weight loss, which has been shown to similar to that seen with calorie restriction
It is true. Energy excess is main reason for fatty liver and diabetes. Obesity is a causative factor for T2D. So weight loss is desirable
(b) Studies on IF show attrition rate of 27-40%
Yes, Some people were unhappy when randomly assigned to undertake IF. Apart from these, dropout rates in controls and IF groups were similar.
(c) Studies have reported that IF is as good as regular calorie restriction but not better
No one has actually claimed that IF is better than regular calorie restriction. It is being mentioned as a more convenient and doable option.
(d) Medication adjustment for diabetic patients has been only recently proposed
Nothing against that. Yes it has been.
(e) Only seven studies have been published regarding patients with T2D of which five were randomised clinical trials and follow up duration has been 4 months or less. All studies reported weight loss and most also reported decline in HbA1c, improvement in glucose, quality of life and blood pressure.
Thats fair amount of evidence. All this evidence is in favour of IF rather than against it.
(f) Only one study has specifically studied hypoglycaemia and in this study fasting led to increased hypoglycaemic episodes
The study mentioned had no control diabetic population that was not fasting. Just comparison of two regimens of fasting. Hypoglycaemia was reported on basis of glucose monitoring when sugar levels dropped below 72 mg/dl. Nearly 60% patients had no recordable event below this levels. One such monitoring event was observed once in 37 days of fasting and once in 75 days of non-fasting. There were no reports of clinically relevant or severe hypoglycaemia that required extra feeding of glucose. Clinical relevance of these findings is unclear at present.
(g) Intermittent fasting could result in wide fluctuations in blood glucose levels
These are doubts expressed without any data observed to support it
References
(i) Horne BD, Grajower MM, Anderson JL.Limited Evidence for the Health Effects and Safety of Intermittent Fasting Among Patients With Type 2 Diabetes. JAMA. 2020;324(4):341–342. doi:10.1001/jama.2020.3908
(ii) Horne BD, Muhlestein JB, Anderson JL. Health effects of intermittent fasting: hormesis or harm? A systematic review. Am J Clin Nutr. 2015;102(2):464-470.doi:10.3945/ajcn.115.109553.
Doesn’t skipping bfast cause gallstones?
What if the evidence flips in 5 years and a whole lot of us end up with such unhealthy side effects?
Also, all old people who observed fast also had other habits that contributed to well being – like waking up early and going for morning varjish/walk and eating Dalia for bfast and not having any junk food.
These are all confounding factors.
Meal skipping has been in vogue for a long time and across various cultures. It is usually acquired from mothers or friends.(i) Does it cause gall stones? I could not find any scientific evidence for this question. Though I did find statements to that effect at many websites.(ii, iii) Actually medical studies do no mention this association at all. Only association of IF that is described, is with higher BMI if children skip breakfast.(iv, v) Skipping breakfast may lead to weight gain in school children, as there is compensatory over-eating later in the day.(vi, vii) Gallstones have been linked to rapid weight-loss for example after bariatric surgery.(viii) There are also studies that show that breakfast skippers have better health related quality of life scores and lower levels of stress/depression as compared to those who ate poor quality breakfast.(ix)
Association between IF and weight-loss, improvement in diabetes, and fatty liver is based on carefully conducted randomised controlled trials. The talk about its long term safety is based on folklore that it was a habit among several generations that ate only two meals a day. No one can guarantee that if you use IF, gallstones will not develop! Just as no one can guarantee that gall stones will not develop if you don’t use IF. (The risk of gallstones may be higher in obese persons)
Your point about other healthy habits is well taken, but at present there are no answers. There is always the option of 30% calorie reduction in all meals, which is equally effective!
References
(i) Pearson N, Williams L, Crawford D, Ball K. Maternal and best friends’ influences on meal-skipping behaviours. Br J Nutr. 2012;108(5):932-938. doi:10.1017/S000711451100612X
(ii) https://www.medicaldaily.com/everyday-practices-will-help-prevent-gallstone-attacks-247598,
(iii) https://www.lybrate.com/topic/is-skipping-meal-actually-the-risk-of-gallstones/e3a7847a264b8b70545bbef8458d0140
(iv) Zilberter T, Zilberter EY. Breakfast: to skip or not to skip?. Front Public Health. 2014;2:59. Published 2014 Jun 3. doi:10.3389/fpubh.2014.00059
(v) Alsharairi NA, Somerset SM. Skipping breakfast in early childhood and its associations with maternal and child BMI: a study of 2-5-year-old Australian children. Eur J Clin Nutr. 2016;70(4):450-455. doi:10.1038/ejcn.2015.184
(vi) Zilberter T, Zilberter EY. Breakfast: to skip or not to skip?. Front Public Health. 2014;2:59. Published 2014 Jun 3. doi:10.3389/fpubh.2014.00059
(vii) Alsharairi NA, Somerset SM. Skipping breakfast in early childhood and its associations with maternal and child BMI: a study of 2-5-year-old Australian children. Eur J Clin Nutr. 2016;70(4):450-455. doi:10.1038/ejcn.2015.184
(viii) McCrory MA. Meal skipping and variables related to energy balance in adults: a brief review, with emphasis on the breakfast meal. Physiol Behav. 2014;134:51-54. doi:10.1016/j.physbeh.2014.05.005.
(ix) Ferrer-Cascales R, Sánchez-SanSegundo M, Ruiz-Robledillo N, Albaladejo-Blázquez N, Laguna-Pérez A, Zaragoza-Martí A. Eat or Skip Breakfast? The Important Role of Breakfast Quality for Health-Related Quality of Life, Stress and Depression in Spanish Adolescents. Int J Environ Res Public Health. 2018;15(8):1781. Published 2018 Aug 19. doi:10.3390/ijerph15081781
Compliments and appreciation on your commendable articulation of the huge benefits of IF, Sir.
Your signature style & super scientific content are a quantum value addition to one’s perspective.
Also love the repartee between the’ father- daughter.
Profound regards to you and Ma’am
As always, sir, you have brought out facts in an easy to understand format. The article and the responses thereto were a pleasure to read
Thank you