“What's in a name? That which we call a rose by any other name would smell just as sweet.” --William Shakespeare In Romeo and Juliet
Another flight
“Sir, may I give you 27C, an aisle seat?” Check-in counter officer at the airlines asked me.
“I would prefer a seat somewhere in the front, if that is possible.” was my request.
His eyes searched around a bit on his computer screen and then he asked, “Sir, only a middle seat is available in the fifth row. Is that all right?”
I nodded and got 5E.
It basically meant that I will be wearing a PPE kit, in addition to the mask and the face shield. When I entered the aircraft dressed as an alien, I noticed that my seat was between two people with big tummies, who were leaning over my seat to chat with each other.
When I reached near my seat, the person on the aisle seat, pointed at the man on the window seat and growled in a very gruff voice,”We are doctors and close friends. Would you allow us to be seated together? We would like to talk to each other. You can take the window seat if you wish.”
Before I could happily accept this offer, the air hostess standing right behind me, announced in a very stern voice, “Sir, you can not change seats due to COVID-19 restrictions.” Then addressing me she added,”Sir. you will have to sit in the middle seat.”
And so that was it. After this, I had to listen to a running conversation across my seat between the gruff voice on my left and a high pitched voice from the seat on my right.
The conversation did interest me, but I decided that I will not look at their faces or interject. It went somewhat like this
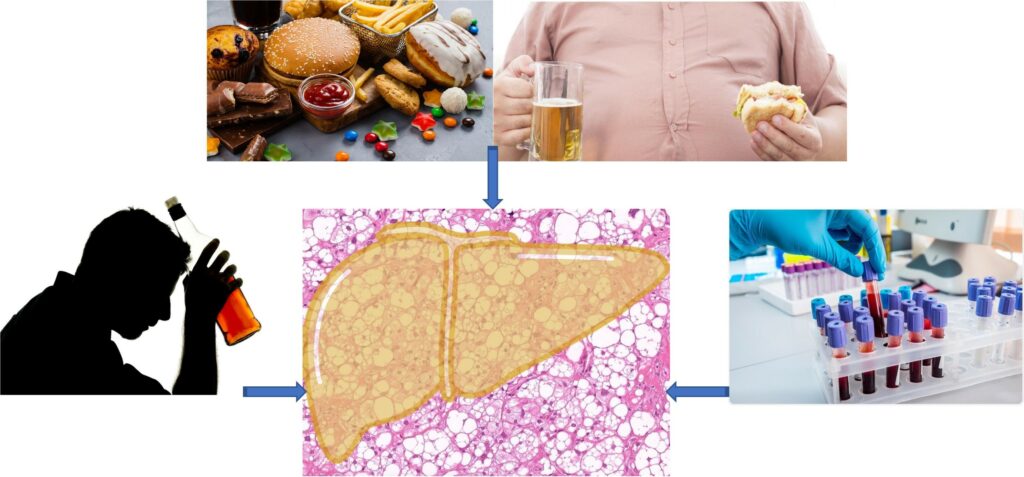
Alcohol as a cause of fatty liver
Gruff voice: “About four decades back, when I did my Gastroenterology training, fatty liver meant alcohol related liver disease (ALD).”
High pitched voice, “Yeaah! I remember, out tutors used to tell us – Don’t use the word alcohol.” There is social stigma attached to it. Use the terms like “ethanol or ‘C2H5OH” in front of patients and relatives, so that patients are spared embarrassment in front of others.”
It was clear that I was among the gastroenterologists. I did not know them personally and hence, from here on, I will use the names GV for gruff voice and HPV for the high pitched voice.
GV: “Fatty liver was a known precursor to alcoholic steato-hepatitis (ASH) and cirrhosis. Alcoholic liver disease accounted for half the deaths from end-stage liver disease (ESLD) in western countries back then.1 And we had no clue about Indian statistics then.”
Alcoholism – a self inflicted disease?
HPV: “Do you remember an interesting point? Those day ALD patients were not considered eligible for liver transplantation when they had liver failure. ALD was considered a self-inflicted disease. One feared that after transplantation, such a person will damage the transplanted liver by drinking more (Transplanted liver is considered the most precious gift by another human being).”
GV: “I still believe that. For example, one could cite an imaginary situation where a drunken driver with liver disease runs over a healthy teen. The teen’s parents agree to donate his liver after his death. How many of us would consider that drunken driver to be a suitable candidate to receive that liver?”2
As eligible as any other disease!
HPV: “The world disagrees with you here. You are harsh on them because you do not drink. There was a lot of debate and lobbying in favor of patients with ALD, and finally, a bold decision was taken. The National Institute of Health (NIH) Consensus Conference on Liver Transplantation in 1983 concluded that ALD may be an appropriate indication for OLT, provided the patient is judged likely to abstain from alcohol after transplantation.“3
GV: “Sadly yes! Tell me how many alcoholics will actually give up alcohol? The Health Care Financing Administration in 1991 went on to identify ALD as one of the seven conditions for which it approved payment for liver transplantation, though it recommended a “significant” period of abstinence for alcoholics before undergoing the procedure.”
Six month rule!
And GV continued, “A requirement for 6 months abstinence from alcohol before placement on the transplant waiting list was considered appropriate for patients with alcoholic liver disease. Many people would hide the fact that they surreptitiously did drink.”4
HPV: “And this rule became acceptable to everyone.”31 HPV carried on further, “It did offer some advantages if strictly followed. For example, it allowed a window of opportunity for the liver to stabilize and recover. It also allowed the opportunity to examine the patient’s commitment to abstain from alcohol. This period of abstinence gave enough time for the addiction team to assess the patient and organize support measures. Sometimes it improved the patient’s clinical condition so much so that several of them did not need transplants! Most transplant programs (85%) in the United States required 6 mo of abstinence before transplantation till recently.” 5
GV: “Liver transplant programs in Europe also required pre-transplant abstinence of 6 months to a year. Even UK guidelines proposed that both length and context of abstinence are among factors to be considered in the wider psychosocial assessment.”6
Is it optimum utilisation of scares resource?
GV further said, “The ethical controversy about this issue has kept simmering. There are people who still think like me!”7,8
HPV: “But we need to change with times. Over the years people have started accepting ALD as a normal indication for liver transplantation and the six-month abstinence rule is gradually fading away in many parts of the world. An alcoholic today may not be required to prove that he has the willpower to give up drinking.”9
New kid on the block arrives
GV: “When this debate was still on, around the turn of the century, another disease appeared on the medical horizon and somewhat overshadowed ALD. Remember? Within a short period, it became the commonest liver disease in many parts of the world and also the commonest indication for liver transplantation. Today this ‘non-alcoholic fatty liver disease!’ (NAFLD) affects ~25% of the adult population in most countries, whereas its more serious form non-alcoholic steatohepatitis (NASH) affects 2–3% of the population.”10
HPV: “I think ALD is still very common. But Yes, NAFLD is gradually taking over. Interestingly, this newly recognised disease had to suffer the indignation of a negative nomenclature. It was called ‘non-alcoholic fatty liver (NAFLD)’ It was fatty liver, but not due to alcohol. Really??? If Shahrukh Khan arrived on the Bollywood scene after Amitabh Bachchan, should we call him Non-Amitabh film star?”
What is in a name?
GV: “We do have a precedence in another disease called – Non-Hodgkin’s Lymphoma! We call a lymphoma by an exotic name Hodgkin’s disease after the person who initially described it. All others types are clubbed as non-Hodgkin’s lymphoma. The exact cause of both diseases is not known. They originate in the same organ cells (Lymphoid cells) but their behaviour is different.” 11,12
HPV: “But several people are not happy with this negative nomenclature and want to change it!”
GV: “The term NASH does have some advantages though. In the case of ASH and NASH, the causes of disease are clearly known. Both have a genetic susceptibility. Both are related to excessive intake of a consumable that gives pleasure by tickling the same pleasure center of brain. Sequences of events and complications are similar. One is caused by alcohol, and the other by excessive eating of sugars and fat. ASH improves if one stops drinking. NASH improves if one can cut down on carbs and calories to lose weight.”13
HPV laughed: “If they are so similar, why the scientists never thought of prescribing a time limit for NASH-cirrhosis patients to lose weight before listing for transplantation. It is well known that losing weight by 10% will lead to significant improvement or even cure in this disease.”
Human behaviour
GV: “Yes, no one has ever thought of a six month rule for NASH. Isn’t that strange? In fact surgeons sometimes offer bariatric surgery for obesity along with transplantation. Both diseases are curable to some extent by altering human behavior. But ultimate treatment ironically, is surgery. An alcohol-related name – NASH is what reminds us that it is also the result of our own indiscretion!
Both GV and HPV were blissfully unaware of their own bulging tummies, while avidly guzzling the snacks offered by the airlines.
HPV: “The medical fraternity knows full well that it is preventable and curable by a simple behavioral change. None the less, it is frantically looking for new medicines that would improve it by barely 20% or so. The pharmaceutical industry is ploughing billions of dollars to find a pill for these self created ills, as you may like to call.”
GV: ” I heard that effort is on to remove the mention of ‘alcohol’ in the name of NASH. An international expert consensus document suggested new criteria for this disease under a new name – metabolism associated fatty liver disease (MAFLD) and metabolism associated steatohepatitis (MASH) for its more serious form.”14
New Definition, new name!
HPV: “I have also read it. In contrast to NAFLD, alcohol consumption will be allowed in this new entity. All one needs to fit into this definition is evidence of fatty liver, along with one of the three criteria, namely, overweight/obesity, presence of type 2 diabetes mellitus [T2DM], or evidence of metabolic dysfunction. The latter was further defined as the presence of any two of the following abnormalities:
a) Waist circumference (WC) >102 and 88 cm in Caucasian men and women, respectively (or >90 and 80 cm in Asian men and women, respectively).
b) Blood pressure >130/85 mm Hg or specific drug treatment.
c) Plasma triglycerides >150 mg/dL or specific drug treatment.
d) Plasma high-density lipoprotein cholesterol <40 mg/dL for men and <50 mg/dL for women or specific drug treatment.
e) Prediabetes (i.e., fasting glucose levels 100–125 mg/dL, or 2-h postload glucose levels 140–199 mg/dL or HbA1c 5.7%–6.4%).
f) Homeostasis model assessment of insulin resistance score >2.5.
g) Plasma high-sensitivity C-reactive protein level >2 mg/L.”
Will this rose with a different name smell as sweet?
GV: “You seem enthusiastic about the new name, but I am not. In medicine, language matters and the words used to name and describe a disease can have a profound impact on patients and their families. Fatty liver is known to science since the 1830s;15 It was known to be associated with obesity and was shown to progress to cirrhosis in a diabetic patient. It took 150 years (finally in 1980) for it to be given a name i.e. NAFLD and NASH.”16
HPV: “Well, I am happy with this new name, i.e., MASH. It has solved a problem of overlap between ASH and NASH”
GV: “How come?”
How much alcohol can NAFLD have?
HPV: “In cold countries where alcohol intake was very common, NAFLD could be diagnosed in patients who took minimal amounts of alcohol acceptable during social interactions. But there is no unanimity about this minimal amount? Suggested thresholds of alcohol consumption have varied from ≤1 drink (14 g) per day to 2-3 drinks [(<30 g) in men and <20 g/day for women].”17,18,19
GV: “So?”
HPV: “You see, studies have also shown that there is no safe limit for alcohol use.”20
NASH may be ASH?
GV: “I am aware of that fact.”
HPV: ” So, this kind of threshold prescribed for diagnosis of NASH, somehow blurred the difference between ASH and NASH! Fatty liver does occur even in complete teetotallers and is often associated with metabolic syndrome. Fact remains that many obese diabetic patients can also be alcohol dependent. So, what will you call the fatty liver in an obese diabetic with heavy alcohol intake? ASH or NASH?”
GV: “Alcohol may not be the only blurring fact. More recently, two additional common factors were discovered which further blurred the difference between ASH and NASH. One was genetic susceptibility and the other was gut microbiota changes, which are commonly seen in most with disease progression.”21
Enter ‘MASH’
HPV: “Then you should be happy with the new name. It comes after several years of debate, and from a consensus meeting of experts to address this need after applying a carefully designed Delphi method.”22
GV: “No, I was quite happy with the older NAFLD and NASH.”
HPV: “The renaming of NAFLD to MAFLD (And NASH to MASH) holds a promise to circumvent the inappropriate and inadvertent consequences of the older term NAFLD, such as stigmatization, trivialization and lack of patient awareness.”
GV: “You talk of stigmatisation? Despite the fact that every fourth person on the Earth may have it, general practitioners, as well as lay people, are singularly unaware of it and its consequences. For example, a recent study indicated that NAFLD is under-recognized and is commonly discovered incidentally at an advanced stage with cirrhosis.”23
and does not squarely point at the individual for having consumed more than appropriate
Blissfully unaware
HPV: “So?”
GV: “People are blissfully unaware about what is happening. Studies tell us that awareness of NAFLD was 1.5%, 2.4%, 2.2% and 3.5%, across the chronological surveys from 2001- 2004, 2005-2008, 2009-2012 and 2013-2016 respectively.24 You change a name that was in use for nearly half the century, it will leave people more confused.”
HPV: May be a change in name will give it more media coverage and more people may get to know about it!”
GV: ” Personally I think this change will not be acceptable. Doctors are notoriously opinionated as well as fickle minded. A recent study that included 482 gastroenterologists and hepatologists mainly from academic centers indicated that in clinical practice, hardly any one follows the consensus guidelines. “25
HPV: “Practice is different when compared to accepting a name. The academic societies of several countries have already accepted it.”
Back seat driver
GV: “Huh! You will be surprised to know that many experts who voted for consensus in the academic meeting, started speaking against it as soon as they came out of the academic atmosphere. Now no one wants a premature change in nomenclature.”26
HPV: “Why should that happen?”
GV: “The changing stance of experts is not exactly puzzling. The powerful research community is funded mostly by the pharmaceutical industry and the latter have a clear conflict of interest. They have, after all, billions of dollars stuck in drug development and in seeking regulatory approval for new drugs developed for NAFLD. If the disease definition changes, they may have to start all over again, right from the beginning! Once MAFLD is defined differently from NAFLD, drugs being approved for the latter can not be approved for the former!”
HPV: “Oh, I see!”
GV: “This murky affair adds to instances which make people accuse that ‘academic medicine is for sale!”27
Academic medicine is for sale!
Sitting there on the middle seat, I was wondering if I had heard those words anywhere? This question was raised two decades back in an editorial ‘Is academic medicine for sale?’ by Angell.28. People had responded to it in different ways. Two published letters may be considered symbolic of doctors’ opinion. One response from Catherine Diamound, says ‘These days, everything is for sale’ while another by Thomas J. Ruane, disagreed ‘No. The current owner is very happy with it.’ 29
Naming a disease is a minor matter for the medical profession. Are we free to do it? Pharmaceutical company already decides what research will be done, and what will be published. They also remotely control what majority of us will prescribe.30 We often talk very casually and often gleefully about this subject, but it may be one of the biggest obstacle to development of medical science. A science that may be required to treat us when we are ill tomorrow. We will be treated according to the dictates of pharmaceutical Industry as it suits them, rather than on the basis of what we need.
Note: The characters are imaginary but the content of conversation is real
References
| ↑1 | McCullough AJ. Alcoholic liver disease. In: Schiff ER, Sorell MF, Maddrey WC, editors. Schiff’s disease of the liver. Philadelphia: Lippincott Williams & Wilkins; 1999. pp. 941–971. |
| ↑2 | Moss AH, Siegler M. Should alcoholics compete equally for liver transplantation? JAMA. 1991 Mar 13; 265(10):1295-8. |
| ↑3 | Lucey MR. Liver transplantation in the alcoholic patient. In: Maddrey WC, Schiff ER, Sorell MF, editors. Transplantation of the liver. Philadelphia: Lippincott Williams & Wilkins; 2001. pp. 319–326. |
| ↑4 | Lucey MR, Brown KA, Everson GT, Fung JJ, Gish R, Keeffe EB, Kneteman NM, Lake JR, Martin P, McDiarmid SV, Rakela J, Shiffman ML, So SK, Wiesner RH. Minimal criteria for placement of adults on the liver transplant waiting list: a report of a national conference organized by the American Society of Transplant Physicians and the American Association for the Study of Liver Diseases. Liver Transpl Surg. 1997 Nov; 3(6):628-37. |
| ↑5 | Everhart JE, Beresford TP. Liver transplantation for alcoholic liver disease: a survey of transplantation programs in the United States. Liver Transpl Surg. 1997 May; 3(3):220-6. |
| ↑6 | Varma V, Webb K, Mirza DF. Liver transplantation for alcoholic liver disease. World J Gastroenterol. 2010;16(35):4377-4393. doi:10.3748/wjg.v16.i35.4377. |
| ↑7 | Benjamin M. Transplantation for Alcoholic Liver Disease: The Ethical Issues. Liver Transplantation and Surgery, Vol 3, No 3 (May), 1997: pp 337-342. |
| ↑8 | Mellinger JL, Volk ML. Transplantation for Alcohol-related Liver Disease: Is It Fair?. Alcohol Alcohol. 2018;53(2):173-177. doi:10.1093/alcalc/agx105. |
| ↑9 | Zambrano A. Why Alcoholics Ought to Compete Equally for Liver Transplants. Bioethics. 2016 Nov; 30(9):689-697. |
| ↑10 | Adams LA, Lymp JF, St Sauver J. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology.2005;129:113–121. |
| ↑11 | https://www.nccn.org/professionals/physician_gls/pdf/b-cell.pdf |
| ↑12 | https://en.wikipedia.org/wiki/Non-Hodgkin_lymphoma |
| ↑13 | Scaglioni F, Ciccia S, Marino M, Bedogni G, Bellentani S. ASH and NASH. Dig Dis. 2011;29(2):202-10. doi: 10.1159/000323886. Epub 2011 Jul 5. PMID: 21734385. |
| ↑14 | Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73:202–209. |
| ↑15 | Addison T. Observations on fatty degeneration of the liver. Guys Hosp Rep. 1836; 1(476): 485. |
| ↑16 | Fouad Y, Waked I, Bollipo S, Gomaa A, Ajlouni Y, Attia D. What’s in a name? Renaming ‘NAFLD’ to ‘MAFLD’. Liver Int. 2020 Jun;40(6):1254-1261. doi: 10.1111/liv.14478. Epub 2020 Apr 28. PMID: 32301554. |
| ↑17 | Siddiqui MS, Harrison SA, Abdelmalek MF, et al. Case definitions for inclusion and analysis of endpoints in clinical trials for nonalcoholic steatohepatitis through the lens of regulatory science. Hepatology. 2018;67(5):2001-2012. |
| ↑18 | Wong VW, Chan WK, Chitturi S, et al. Asia-Pacific working party on non-alcoholic fatty liver disease guidelines 2017-part 1: definition, risk factors and assessment. J Gastroenterol Hepatol. 2018;33(1):70-85. |
| ↑19 | Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328-357. |
| ↑20 | GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018 Sep 22;392(10152):1015-1035. doi: 10.1016/S0140-6736(18)31310-2. Epub 2018 Aug 23. Erratum in: Lancet. 2018 Sep 29;392(10153):1116. Erratum in: Lancet. 2019 Jun 22;393(10190):e44. PMID: 30146330; PMCID: PMC6148333. |
| ↑21 | Yuan J, Chen C, Cui J, et al. Fatty liver disease caused by high-alcohol-producing Klebsiella pneumoniae. Cell Metab. 2019;30(6):1172. |
| ↑22 | Eslam M, Sanyal AJ, George J. Toward more accurate nomenclature for fatty liver diseases. Gastroenterology. 2019;157(3):590-593. |
| ↑23 | Bertot LC, Jeffrey GP, Wallace M, et al. Nonalcoholic fatty liver disease-related cirrhosis is commonly unrecognized and associated with hepatocellular carcinoma. Hepatol Commun. 2017;1(1):53-60. |
| ↑24 | Singh A, Kumar A, Singh S, et al. Trends of awareness of the non-alcoholic fatty liver disease, alcoholic liver disease and both fatty liver diseases (BAFLD) using national health and nutrition examination survey: 836. Am J Gastroenterol. 2018;113:S465. |
| ↑25 | Rinella ME, Lominadze Z, Loomba R, et al. Practice patterns in NAFLD and NASH: real life differs from published guidelines. Therap Adv Gastroenterol. 2016;9(1):4-12. |
| ↑26 | Younossi, Z.M., Rinella, M.E., Sanyal, A.J., Harrison, S.A., Brunt, E.M., Goodman, Z., Cohen, D.E. and Loomba, R. (2021), From NAFLD to MAFLD: Implications of a Premature Change in Terminology. Hepatology, 73: 1194-1198. https://doi.org/10.1002/hep.31420 |
| ↑27 | Angell M. Is academic medicine for sale? N Engl J Med. 2000 May 18;342(20):1516-8. doi: 10.1056/NEJM200005183422009. PMID: 10816191. |
| ↑28 | Angell M. Is academic medicine for sale? N Engl 1 Med 2000;342:1516-18. |
| ↑29 | Correspondence. Is academic medicine for sale? N Engl J Med 2000;343:508-10. |
| ↑30 | Anand AC. The pharmaceutical industry: our ‘silent’ partner in the practice of medicine. Natl Med J India. 2000 Nov-Dec;13(6):319-21. PMID: 11209490. |
| ↑31 | Anand AC, Ferraz-Neto BH, Nightingale P, Mirza DF, White AC, McMaster P et al. Liver transplantation for alcoholic liver disease: evaluation of a selection protocol. Hepatology 1997; 25(6):1478-1484. |
Be First to Comment